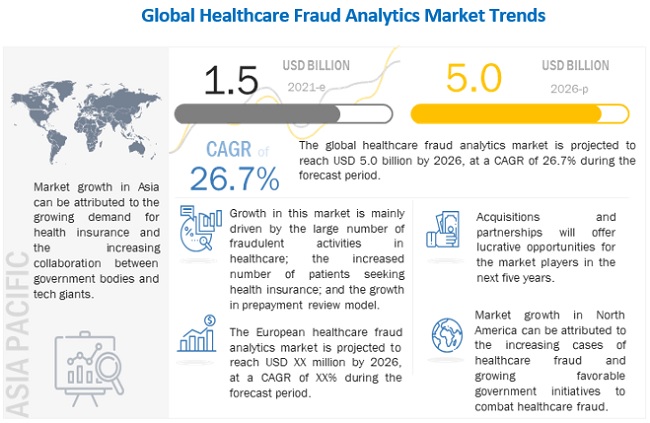
The global healthcare fraud analytics market in terms of revenue was estimated to be worth $1.5 billion in 2021 and is poised to reach $5.0 billion by 2026, growing at a CAGR of 26.7% from 2021 to 2026.
Market growth can be attributed to a large number of fraudulent activities in healthcare, an increasing number of patients seeking health insurance, high returns on investment, and the rising number of pharmacy claims-related frauds. However, the dearth of skilled personnel is expected to restrain the growth of this market.
The number of people utilising various healthcare programmes has increased significantly over the years.
The ageing population, increased healthcare expenditure, and increased disease burden are all factors contributing to the growth of the health insurance market. In the US, the number of citizens without health insurance has significantly decreased, from 48 million in 2010 to 28.6 million in 2016. In 2017, 12.2 million people signed up for or renewed their health insurance during the 2017 open enrollment period (source: National Center for Health Statistics).
According to the new market research report "Healthcare Fraud Analytics Market by Solution Type (Descriptive, Predictive, Prescriptive), Application (Insurance Claim, Payment Integrity), Delivery (On-premise, Cloud), End User (Government, Employers, Payers), COVID-19 Impact - Global Forecast to 2026", is projected to reach USD 5.0 billion by 2026 from USD 1.5 billion in 2021, at a CAGR of 26.7% during the forecast period.
Browse in-depth TOC on "Healthcare Fraud Analytics Market"
155- Tables
32- Figures
176- Pages
Download PDF Brochure: https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
Based on end user, the healthcare fraud detection market is segmented into public & government agencies, private insurance payers, employers, and third-party service providers. The public & government agencies segment accounted for the largest share of the healthcare fraud analytics market in 2019. The increasing cost burden due to healthcare fraud is proving to be a financial threat to public and government agencies globally. These factors are compelling payer organizations associated with these agencies to adopt analytics solutions to avoid losses incurred due to FWA and improper payments, which is driving the market growth.
Geographical Growth Scenario:
The North American healthcare fraud analytics market is expected to grow at the highest CAGR from 2021 to 2026. Factors such as the high number of cases of healthcare fraud, including pharmacy-related fraud, favorable government initiatives, technological advancements, and the availability of solutions in this region are expected to drive the growth of the North American market during the forecast period.
Major players in this market include IBM Corporation (US), Optum, Inc. (US), Cotiviti, Inc. (US), Change Healthcare (US), Fair Isaac Corporation (US), SAS Institute Inc. (US), EXLService Holdings, Inc. (US), Wipro Limited (India), Conduent, Incorporated (US), CGI Inc. (Canada), HCL Technologies Limited (India), Qlarant, Inc. (US), DXC Technology (US), Northrop Grumman Corporation (US), LexisNexis (US), Healthcare Fraud Shield (US), Sharecare, Inc. (US), FraudLens, Inc. (US), HMS Holding Corp. (US), Codoxo (US), H20.ai (US), Pondera Solutions, Inc. (US), FRISS (The Netherlands), Multiplan (US), FraudScope (US), and OSP Labs (US).



