Anastomosis Devices: Enabling Minimally Invasive Surgeries
Anastomosis devices are emerging as an important surgical technology facilitating minimally invasive surgeries in modern healthcare. Anastomosis refers to the surgical joining of two hollow structures, like blood vessels or intestines. While traditionally anastomoses were performed manually using surgical sutures and knots, the advent of anastomosis devices now enables surgeons to perform these complex tasks in a minimally invasive manner through small incisions or even through natural openings like the mouth. This article explores the working, advantages and future promise of anastomosis devices in surgery.
Types of Anastomosis Devices
Anastomosis devices come in different types depending on the specific applications in surgery. Some common types include:
- Circular staplers: These are used to join sections of the intestine or bowel in gastrointestinal surgeries. Circular staplers expedite intestinal anastomoses during procedures like bowel resection or surgery for inflammatory bowel disease.
- Linear staplers: Used in vascular surgery to join cut blood vessels, linear staplers help in creating minimally invasive arterial or venous anastomoses.
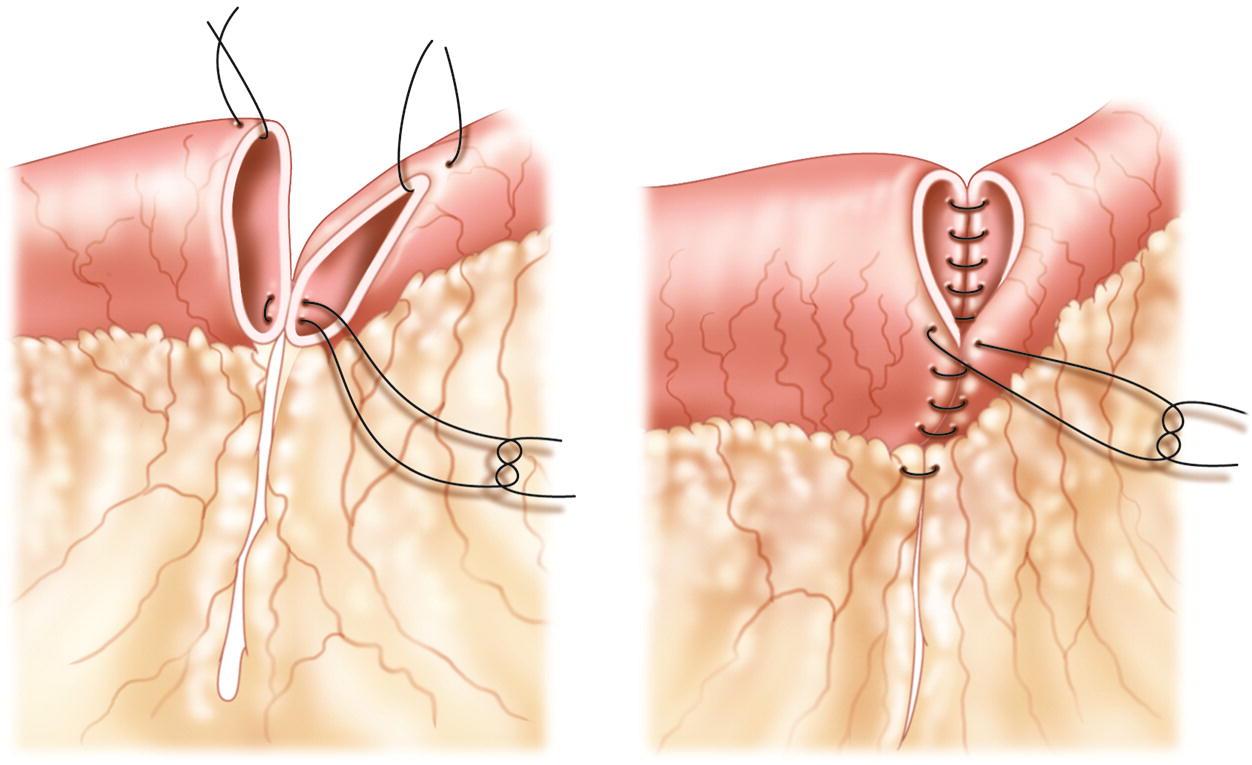
- Suturing devices: Some anastomosis devices rely on precise robotic or computer-controlled suturing instead of stapling. These are used where tissue strength needs to be maximized.
- Adhesive/sealant applicators: Specialized devices are being developed to apply surgical adhesives or sealants instead of staples or sutures for some anastomoses.
Advantages of Anastomosis Devices
The usage of anastomosis devices brings several advantages compared to manual anastomoses:
Precision and reproducibility: Devices enable a consistent, calibrated anastomosis every time with well defined parameters like staple height. This ensures uniform results.
Speed: Automated devices can join tissue, blood vessels or bowel significantly faster than manual suturing. This speeds up surgeries.
Accuracy in MIS: Anastomoses can be performed through small ports with camera guidance, enabling minimally invasive procedures for conditions earlier addressed through open surgeries only.
Reduced complications: Properly placed and applied staple or suture lines result in fewer leakage issues compared to hand-sewn anastomoses. This also translates to shorter hospital stays.
Learning curve: Unlike manual suturing, Anastomoses Devices have shallow learning curves allowing surgeons to achieve consistent results quickly after a short training period.
Future directions
Research into anastomosis devices is ongoing to address tougher clinical scenarios:
Robotic integration: Next-gen devices will incorporate robotics and precision motion control for even finer anastomoses through natural openings like in transoral surgery.
Tissue-specific models: Customizable devices tailored for different tissue properties like thickness, strength and elasticity of intestines, blood vessels or ureters are under development.
Energy-based methods: Non-stapling techniques relying on advanced tissue welding, fusion or adhesion technologies show promise, especially for minimally invasive procedures.
Single-use devices: Disposable, single-use variants aim to reduce the risk of infection in addition to cutting sterilization costs per procedure compared to reusable instruments.
In summary, anastomosis devices present a transformative technology in modern surgery by enabling minimally invasive approaches for complex reconstructive tasks earlier feasible only through open surgeries. Continued innovations promise to make their usage even more refined and applicable to an ever wider range of clinical problems.
For more Insights, Read –
https://www.insightprobing.com/anastomosis-devices-trends-size-and-share-analysis/
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Giochi
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Altre informazioni
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
- IT, Cloud, Software and Technology


