Blood-Based Biomarker: A Cutting-Edge Approach to Non-Invasive Disease Detection
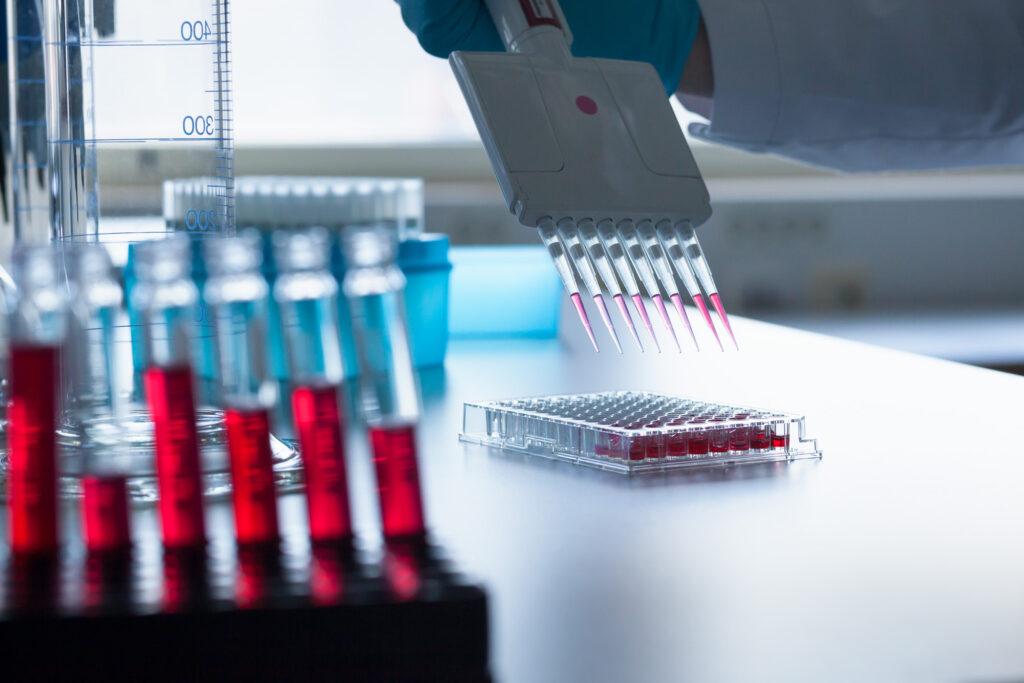
A biomarker is defined as a measurable indicator of some biological state or condition. In healthcare, biomarkers can be utilized to detect and monitor diseases, as well as gauge treatment responses. Traditional biomarkers have often involved invasive procedures like tissue biopsies to obtain samples. However, blood-based biomarkers offer a highly appealing alternative thanks to the non-invasive nature of blood collection.
Advantages of Blood-Based Biomarkers
There are several key advantages to developing Blood Based Biomarkers over traditional tissue-based ones. First, blood samples can be easily, safely, and repeatedly obtained from patients via routine blood draws. This eliminates risks associated with invasive biopsy procedures and allows for longitudinal monitoring over time. Second, blood flows through and in contact with virtually every organ system in the body. As a result, blood serves as an ideal “biosource” for capturing molecular changes indicative of diseases occurring systemically or locally. Third, biomarkers found in blood are generally more amenable to standardization in clinical testing compared to biomarkers from variable tissue sources. Finally, blood collection and processing are well-established procedures making blood-based biomarkers highly translatable into clinical practice.
Discovery of Novel Blood Biomarkers
Modern “omics” technologies like proteomics, metabolomics, and genomics have vastly expanded opportunities for discovering novel blood-based biomarkers. Proteomics uses mass spectrometry and immunoassays to characterize protein expression profiles in blood which can reflect active biological pathways and disease states. Metabolomics analyzes small molecule metabolites in blood that are end-products of cellular biochemical reactions. Changes in metabolite levels result from genetic variations or environmental exposures like infections and cancers. Genomics evaluates circulating cell-free DNA, RNA, and exosomes shed from tissues for disease-associated genetic and epigenetic alterations. These multi-dimensional datasets allow comprehensive molecular phenotyping from blood to pinpoint signatures of disease mechanisms and progression.
Example Blood Biomarkers in Oncology
Cancer diagnostics and monitoring have greatly benefited from blood-based biomarker development. For example, prostate-specific antigen (PSA) testing uses a protein biomarker in blood for prostate cancer screening and recurrence monitoring. Carcinoembryonic antigen (CEA) levels track the response of colorectal cancer to treatment. More recently, liquid biopsies analyzing circulating tumor DNA have shown promise for detecting mutation profiles of cancers from blood to guide personalized therapies. Advanced biomarker panels using proteomics and metabolomics hold potential for earlier detection of cancers before clinical signs emerge as well as real-time surveillance of metastatic spread or residual disease. Efforts are also underway to develop blood biomarkers for predicting immunotherapy responses in various cancers.
Blood Biomarkers for Neurodegenerative Diseases
Blood-based approaches hold promise for improving diagnosis and monitoring of neurodegenerative conditions which traditionally rely on invasive brain biopsies or post-mortem examinations. For Alzheimer’s disease, concentrations of amyloid-β and tau proteins in blood show correlation with brain pathology and may predict progression from mild cognitive impairment to dementia. Other candidates under study include inflammatory markers, neuronal injury biomarkers, and lipid/metabolite signatures linked to neurodegeneration. Biomarkers are also being investigated for concussions/traumatic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, and prion diseases using blood sampling. Non-invasive biomarker testing could enable earlier and more accurate diagnosis, aid drug development through monitoring treatment responses, and advance understanding of disease mechanisms in neurodegeneration.
Regulatory Considerations and Future Outlook
For blood based biomarker to achieve clinical utilization, rigorous analytical and clinical validation studies are required to demonstrate adequate performance specifications for intended applications per regulatory agency guidelines. Assay reproducibility, accuracy, sensitivity, specificity, and establishment of appropriate clinical cut-off criteria are crucial evaluation metrics. Large prospective longitudinal clinical cohort studies are also important to verify biomarker abilities to predict or associate with clinical outcomes over time in target patient populations. Despite inherent technical challenges, the non-invasive nature of blood sampling makes validation and regulatory approval of qualified blood biomarkers an appealing prospect. Ultimately, multi-analyte biomarker panels tailored for specific diseases hold the greatest potential to transform healthcare through minimally invasive liquid biopsy testing approaches of the future.
Get more insights on This Topic- Blood Based Biomarker
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
- IT, Cloud, Software and Technology


