What to Look for in Thoracic Outlet Syndrome Symptoms, Why They Vary by Individual, and How to Discuss Them with Your Doctor
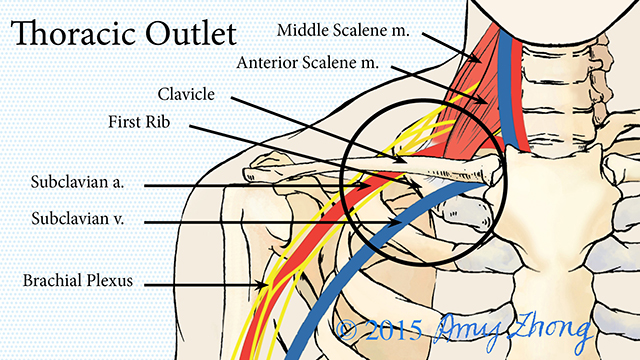
Thoracic Outlet Syndrome (TOS) is a condition that occurs when nerves, veins, or arteries in the thoracic outlet — located between the collarbone and the first rib — are compressed. This compression can result in a wide range of symptoms that vary significantly from one individual to another. Knowing what to look for in TOS symptoms, understanding why they differ, and learning how to effectively communicate these symptoms with your doctor is essential for early diagnosis and appropriate treatment.
Understanding Thoracic Outlet Syndrome
Thoracic Outlet Syndrome is classified into three main types based on the structures being compressed:
Neurogenic TOS: The most common type, neurogenic TOS, occurs when the brachial plexus nerves are compressed. This affects the nerves that control muscle movement and sensation in the shoulder, arm, and hand.
Venous TOS: This type involves the compression of veins, leading to issues related to blood flow from the arm back to the heart.
Arterial TOS: The rarest form, arterial TOS, occurs when the arteries are compressed, affecting blood flow to the arm.
Each of these types presents with unique symptoms, which can further vary depending on the severity of the compression and the individual’s anatomy or lifestyle.
What to Look for in Thoracic Outlet Syndrome Symptoms
Recognizing the symptoms of Thoracic Outlet Syndrome is key to seeking timely medical attention. However, the symptoms can be subtle or mimic other conditions, making self-diagnosis challenging. Here are some common symptoms to look out for, categorized by the type of TOS:
Neurogenic Thoracic Outlet Syndrome Symptoms
As the most prevalent form, neurogenic TOS often presents with neurological symptoms that affect the arm, hand, and sometimes the neck and shoulder. Common symptoms include:
Numbness or tingling: Many individuals experience a tingling sensation or numbness, particularly in the fingers, hand, or forearm. This is often mistaken for carpal tunnel syndrome.
Weakness in the arm or hand: Some individuals find that their grip strength diminishes, making it harder to perform tasks such as lifting objects or writing.
Muscle wasting in the hand: In more severe cases, the muscles at the base of the thumb may shrink due to chronic nerve compression.
Pain in the neck, shoulder, or arm: Pain can range from a dull ache to sharp discomfort, often worsening with activity.
Decreased range of motion: Tightness or stiffness in the shoulder and arm may limit movement, making it difficult to reach overhead or perform repetitive tasks.
Venous Thoracic Outlet Syndrome Symptoms
Venous TOS primarily affects the circulation of blood in the veins. Symptoms related to venous TOS include:
Swelling of the arm or hand: This swelling may appear suddenly, often after physical activity or extended periods of arm use.
Bluish skin discoloration: Due to restricted blood flow, the affected arm or hand may take on a bluish or purplish hue.
Heaviness or aching sensation: The arm may feel heavy or fatigued, even after light activity.
Prominent veins in the shoulder or arm: Some individuals notice that the veins in the shoulder or upper chest become more visible or swollen.
Arterial Thoracic Outlet Syndrome Symptoms
Arterial TOS is less common but can be more severe due to the involvement of the arteries. Symptoms to watch for include:
Coldness in the arm or hand: Restricted blood flow to the extremities may result in a cool or cold sensation in the affected arm or hand.
Weak pulse or no pulse: In extreme cases, individuals may notice a diminished or absent pulse in the wrist or hand.
Paleness or bluish color in the fingers: Fingers may appear pale or discolored due to inadequate blood supply.
Cramping or fatigue during use: Some individuals report cramping or muscle fatigue in the arm when performing routine activities, even those that do not seem physically demanding.
Why Thoracic Outlet Syndrome Symptoms Vary by Individual
Symptoms of Thoracic Outlet Syndrome can vary widely from one person to the next. Several factors contribute to these differences, including the specific type of TOS, the degree of compression, and individual anatomy or lifestyle factors.
1. Type of TOS
As described earlier, the type of TOS (neurogenic, venous, or arterial) largely determines the kind of symptoms an individual will experience. For example, someone with neurogenic TOS is more likely to experience numbness and weakness, while someone with venous TOS may notice swelling or skin discoloration.
2. Severity of Compression
The degree of compression on the nerves, veins, or arteries also influences symptom presentation. Mild compression might lead to intermittent discomfort or tingling, while severe compression can cause more debilitating symptoms, such as muscle wasting, constant pain, or circulatory issues.
3. Individual Anatomy
Some individuals may have anatomical abnormalities that make them more prone to developing TOS. These include having an extra rib (cervical rib), unusually tight muscles, or a narrow thoracic outlet. Variations in anatomy can also affect how symptoms manifest; for example, a cervical rib might compress a nerve in one person, while in another, it compresses an artery.
4. Lifestyle and Activity Level
People who engage in repetitive arm movements, such as athletes or individuals with physically demanding jobs, are more likely to develop TOS. Their symptoms may worsen with activity and improve with rest. In contrast, individuals with a sedentary lifestyle may have different triggers for their symptoms, such as poor posture or long periods of sitting.
How to Discuss thoracic outlet syndrome symptoms with Your Doctor
Effectively communicating your symptoms to your doctor is crucial for an accurate diagnosis and appropriate treatment. Because TOS symptoms can be easily confused with other conditions like carpal tunnel syndrome or cervical spine disorders, it’s essential to provide your doctor with detailed and clear information.
1. Be Specific About Your Symptoms
When discussing your symptoms with your doctor, be as specific as possible. Describe the location, intensity, and duration of your symptoms. Mention any activities or movements that trigger or worsen your symptoms, such as lifting your arms overhead, carrying heavy objects, or typing on a computer.
For example, instead of saying, “I have arm pain,” you could say, “I feel a sharp pain in my shoulder and numbness that radiates down my arm, especially when I lift my arms above my head.”
2. Keep a Symptom Diary
A symptom diary can help your doctor better understand the frequency and severity of your symptoms. Note when the symptoms occur, how long they last, and any factors that seem to relieve or aggravate them. This can help your doctor identify patterns and possible triggers.
3. Discuss Your Medical History and Lifestyle
Your doctor will want to know about any previous injuries, surgeries, or chronic conditions that could contribute to your symptoms. Be sure to mention any trauma to the neck or shoulder area, as well as any repetitive movements related to work or sports. Lifestyle factors such as poor posture or spending long periods at a desk may also be relevant.
4. Ask Questions About the Diagnosis and Treatment
TOS can be difficult to diagnose, so don’t hesitate to ask your doctor about the next steps. Will you need imaging tests or nerve conduction studies? What are the potential treatment options? Understanding the diagnostic process and available treatments will help you feel more informed and empowered.
Conclusion
Thoracic Outlet Syndrome can present with a variety of symptoms, depending on the type and severity of the condition. By knowing what to look for and why symptoms vary from person to person, you can better assess your situation and seek timely medical attention. Clear communication with your doctor is essential for a proper diagnosis and treatment plan. If you suspect you may have TOS, don’t hesitate to take action — early intervention can prevent long-term complications and improve your quality of life.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Jocuri
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Alte
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
- IT, Cloud, Software and Technology


