How Deep Brain Stimulation Is Changing Parkinson’s Treatment
Parkinson’s disease (PD) is a progressive neurological disorder that affects movement, causing tremors, rigidity, bradykinesia (slowness of movement), and postural instability. As the disease advances, it significantly impacts daily life and can be challenging to manage. Although there is no cure for Parkinson's disease, several treatments aim to alleviate symptoms and improve quality of life. Among these treatments, Deep Brain Stimulation (DBS) has emerged as a transformative approach, offering hope and improved outcomes for many patients with Parkinson’s.
What is Deep Brain Stimulation (DBS)?
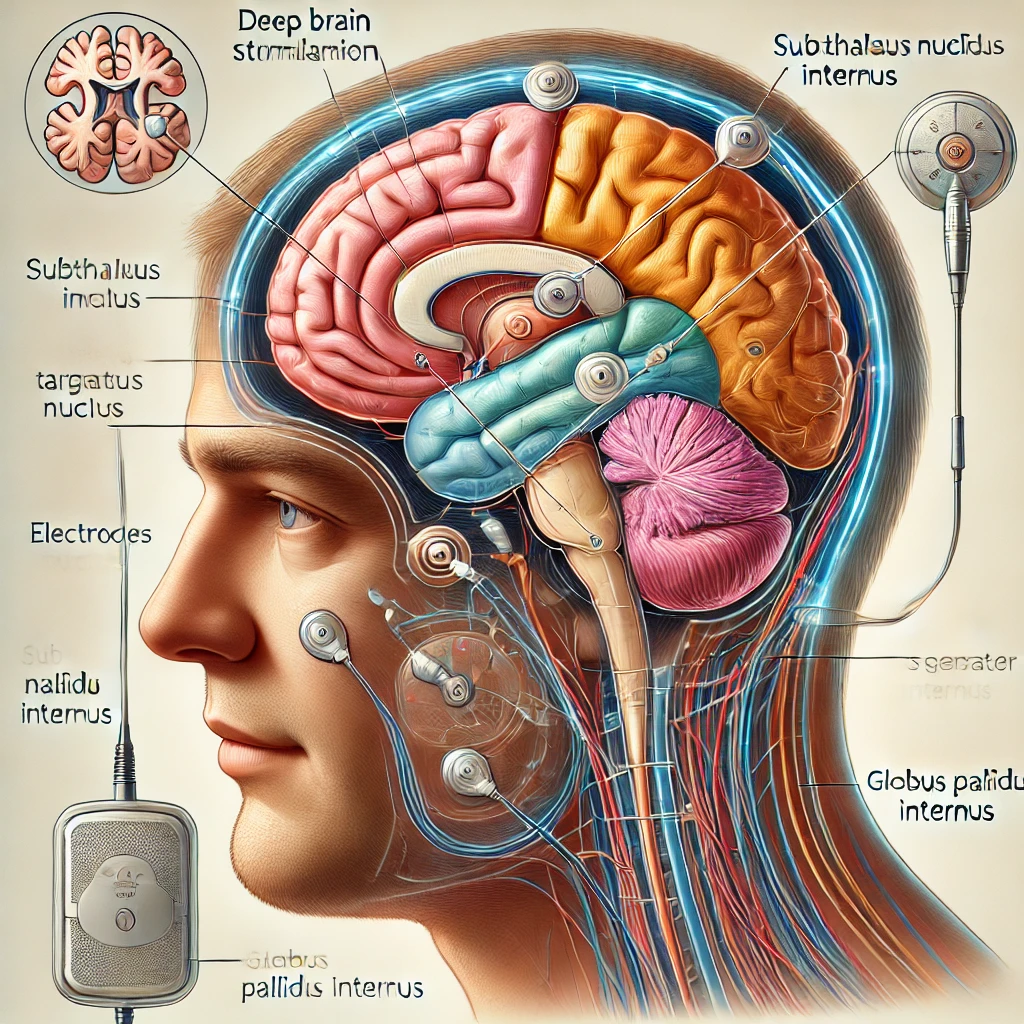
Deep Brain Stimulation is a surgical procedure that involves implanting a small device, similar to a pacemaker, in the brain to regulate abnormal brain activity. DBS is designed to target specific areas of the brain involved in controlling movement. For patients with Parkinson’s, this procedure is typically used to treat motor symptoms that are no longer well-controlled by medication.
DBS involves placing electrodes in the subthalamic nucleus (STN) or globus pallidus internus (GPi), both of which are areas of the brain that regulate movement. These electrodes are connected to a small pulse generator, implanted under the skin in the chest area, similar to a pacemaker. The pulse generator sends electrical impulses to the brain, helping to correct the irregular neural firing patterns that contribute to the symptoms of Parkinson’s.
How Does DBS Work in Parkinson's Disease?
The brain’s movement-related circuits become disrupted in Parkinson’s disease, primarily due to the loss of dopamine-producing cells in the substantia nigra, a key part of the basal ganglia. This leads to an imbalance of activity between different brain regions, resulting in the hallmark motor symptoms of PD.
DBS works by stimulating specific parts of the brain that are involved in controlling movement. By sending electrical impulses to the targeted regions, DBS helps restore the normal patterns of brain activity and improves the brain's ability to communicate with the muscles. The stimulation helps to smooth out the communication between the brain and body, reducing tremors, rigidity, and improving motor control.
Benefits of Deep Brain Stimulation for Parkinson’s Disease
DBS has proven to be an effective treatment for patients with Parkinson’s who have not experienced sufficient symptom relief from medications. Some of the key benefits of DBS in treating Parkinson's disease include:
1. Improved Motor Symptoms
DBS has been shown to provide significant relief from the most common motor symptoms of Parkinson’s disease, including:
- Tremors: Resting tremors, one of the most characteristic symptoms of Parkinson’s, are often reduced or eliminated with DBS.
- Bradykinesia: The slowness of movement can be significantly improved with DBS, allowing patients to move more freely and perform everyday activities with greater ease.
- Rigidity: Stiffness in the muscles is reduced, making it easier for patients to move and maintain flexibility.
- Postural Instability: Although DBS is not a cure for balance problems, it can help improve stability and reduce falls.
Many patients experience a 50% to 70% improvement in motor symptoms after DBS surgery, which can last for several years.
2. Reduced Need for Medications
One of the most significant advantages of DBS is its ability to reduce the reliance on medications, especially levodopa, the mainstay treatment for Parkinson’s. While levodopa is effective at controlling symptoms, it can cause side effects over time, such as motor fluctuations (the “on-off” phenomenon) and dyskinesias (involuntary movements). With DBS, patients often experience more consistent symptom control and may require lower doses of medication, reducing the likelihood of these side effects.
3. Improved Quality of Life
As motor symptoms are controlled, patients report a better quality of life, including the ability to engage in activities that they had previously found difficult or impossible. Daily tasks such as eating, dressing, and walking can become less challenging, allowing individuals to regain a sense of independence and improve overall well-being.
4. Long-Term Efficacy
DBS has been shown to provide long-term benefits for patients with Parkinson’s. While medication may lose its effectiveness over time, DBS can continue to offer symptom relief for 5 to 10 years or more, with adjustments made to the device to accommodate changes in the patient’s condition.
The DBS Procedure
The DBS procedure is typically performed in two stages:
1. Electrode Implantation
The first step involves placing the electrodes in the targeted areas of the brain (usually the subthalamic nucleus or globus pallidus). This is done while the patient is awake, allowing the surgical team to monitor the patient’s response to stimulation. During the surgery, the patient may be asked to perform specific tasks, such as moving their hands or fingers, to assess the effectiveness of the electrode placement in reducing symptoms.
Once the electrodes are placed, they are connected to a pulse generator, which is implanted under the skin near the collarbone or chest. The pulse generator controls the electrical impulses sent to the brain.
2. Programming the Device
After the electrodes are implanted, the DBS device is programmed and adjusted. The patient will undergo a series of follow-up visits where the neurologist fine-tunes the settings to find the most effective stimulation parameters. This may take several months, as adjustments are made to optimize the balance between symptom relief and potential side effects.
Risks and Considerations
While DBS is generally considered a safe and effective treatment for Parkinson’s, like any surgery, it carries risks. Some potential risks include:
- Surgical Complications: As with any brain surgery, there are risks related to anesthesia, infection, or bleeding during the procedure.
- Device Malfunction: The DBS device may malfunction or require adjustments over time, which can lead to changes in symptom control.
- Side Effects of Stimulation: In some cases, DBS may cause side effects such as mood changes, speech difficulties, or tingling sensations. However, these can often be managed with adjustments to the device settings.
- Cognitive and Psychiatric Effects: Some patients may experience cognitive changes, depression, or other psychiatric symptoms, particularly if the stimulation is not carefully calibrated.
Patients must undergo thorough evaluations before being considered for DBS to ensure they are good candidates for the procedure. Factors such as age, overall health, and the progression of Parkinson’s disease will be taken into account.
Who is a Candidate for DBS?
DBS is typically considered for patients with moderate to advanced Parkinson’s disease treatment who have not responded well to medications or who experience significant motor fluctuations and dyskinesias despite optimal pharmacological treatment. Candidates for DBS must meet certain criteria, including:
- Good response to levodopa: The patient should have a history of good response to levodopa therapy, as DBS is most effective when it is used in combination with medication.
- Stable mental health: Patients should be free of major psychiatric conditions, such as severe depression or psychosis, that could be worsened by the procedure.
- Ability to undergo surgery: Patients must be able to tolerate the surgery and anesthesia.
The Future of Deep Brain Stimulation in Parkinson’s Treatment
As technology advances, the future of DBS looks promising. Newer developments include adaptive DBS, which adjusts the stimulation in real time based on brain activity. This type of DBS could provide more precise and personalized treatment, further improving outcomes for patients with Parkinson’s disease. Additionally, researchers are investigating DBS in combination with other therapies, such as gene therapy and stem cell therapy, which may enhance its effectiveness and offer even more options for Parkinson’s patients.
Conclusion
Deep Brain Stimulation has revolutionized the treatment landscape for Parkinson’s disease. For many patients, it offers a significant improvement in motor function, reduces the need for medications, and enhances quality of life. While it is not a cure for Parkinson’s, DBS provides a powerful tool for managing symptoms and improving the daily lives of individuals with the disease. As research continues and technology evolves, the potential for DBS to transform Parkinson’s treatment continues to grow, offering hope for a brighter future for those living with this challenging condition.
If you or a loved one is living with Parkinson’s disease and considering Deep Brain Stimulation (DBS) as a treatment option, it's essential to consult with an experienced and skilled neurosurgeon. Dr. Chirag Solanki, one of the best neurosurgeons in Ahmedabad, specializes in cutting-edge treatments like DBS.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
- IT, Cloud, Software and Technology


